Fibromyalgia is a condition that causes chronic pain throughout the body, fatigue, anxiety, and nerve dysfunction. Today, it affects the life of 4 million people in the US alone and, if left untreated, it can lead to disability. Given that there is no definitive cure for fibromyalgia, treatments primarily aim to ease its symptoms.
Despite how common and debilitating this condition is, its “invisible” nature has led to a delay in the research on its causes, symptoms, and prognosis. Certainly, with clinical trials only starting in the 1980s, a lot is yet to be understood about the nature of fibromyalgia.
However, one emerging hypothesis is that fibromyalgia is an autoimmune disease, which is a condition caused by the immune system mistakenly attacking healthy cells.
This theory hasn’t obtained widespread acceptance by the international scientific community but, if the findings of new research are accurate, it may open new pathways to better understand and treat fibromyalgia.
In this guide, we’ll look at the connection between fibromyalgia and autoimmunity, and how this condition can be addressed without medications or surgery. Let’s dive in.
The Link Between Fibromyalgia And Autoimmunity
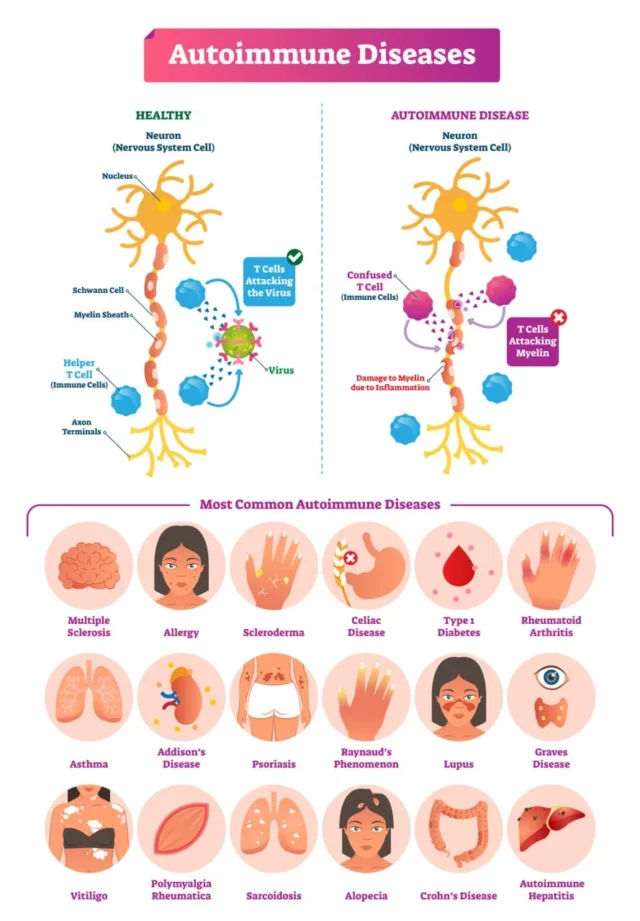
To understand why fibromyalgia may be classified as an autoimmune disease, it is first important to determine what autoimmunity is. Autoimmunity refers to a condition where the immune system fights healthy tissues or cells in the body, mistaking them for pathogens such as viruses and bacteria.
When the immune system attacks those healthy cells, it also causes high levels of sustained inflammation and progressive damage.
Some common autoimmune conditions include Crohn’s disease, type 1 diabetes, rheumatoid arthritis, lupus, and multiple sclerosis. There is no cure for these conditions, and most treatments aim at helping patients manage their symptoms.
To categorize a disorder as an autoimmune disease, certain hallmarks should be present. These include:
- Damage to the body’s tissues caused by the immune system attack
- Sustained inflammation
- Autoantibodies
Autoantibodies are protective proteins produced by the immune system, which mistakenly identify healthy cells in the body as foreign particles, and attack them. There are different types of autoantibodies, and each of them may attack one or more types of cells.
For example, the presence of the autoantibody anti-dsDNA is associated with the development of lupus, while anti-CCP is linked to an increased risk for rheumatoid arthritis.
So, for fibromyalgia to be classified as an autoimmune disease, research must verify the presence of the hallmarks seen above. However, for decades, both the existence and the nature of fibromyalgia were controversial. Due to the lack of adequate diagnostic tools, this condition was classified as “arthritis-like” and described as “generalized musculoskeletal pain”.
However, fibromyalgia has several similarities with autoimmune diseases, including:
- It is more common in women
- It often develops following trauma or disease
- Pathogens like Hepatitis C can increase the risk of suffering from this condition
- It may occur alongside other autoimmune diseases
- It can develop after medical events like vaccinations and silicone breast implant procedures
New research has also shown that, besides similarities with autoimmune diseases, fibromyalgia carries some hallmarks associated with autoimmunity:
- Autoantibodies: The autoantibodies anti 68/48 kDa and anti 45 kDa were found in 15.6% and 37.1% of patients with fibromyalgia, respectively.
- Inflammation: A 2022 study shows that people with fibromyalgia have high levels of 19 inflammatory serum proteins, which are associated with widespread inflammation.
- Damage: Fibromyalgia is often associated with small-fiber neuropathy (damage to nerve fibers).
Lastly, fibromyalgia is characterized by increased pain-related activity in the brain, which is linked to abnormal neuroinflammation, or the inflammation of the central nervous system (the nerves in the brain and spinal cord).
The Role Of Genetics And Immune System Obstruction
Given that the hypothesis that links fibromyalgia to autoimmunity isn’t widely accepted, this chronic pain condition isn’t officially classified as an autoimmune disease. Nonetheless, genetics and the immune system play a significant role in the risk and development of fibromyalgia.
According to a 2021 study, most of the symptoms of fibromyalgia – including fatigue and increased pain sensitivity – are caused by the abnormal increase in the activity of pain-sensing nerves throughout the body
Overactivity in the immune system usually occurs after an infection or injury, and it is caused by the presence of certain antibodies. This connection makes fibromyalgia a disease of the immune system.
Another factor playing a role in fibromyalgia is genetics. Research shows that having a close relative with an autoimmune disease such as rheumatoid arthritis or lupus increases your risk of developing fibromyalgia.
What’s more, according to a study published in the journal Arthritis & Rheumatology, having a first-degree relative with fibromyalgia may increase the risk of developing this condition by 8.5 times.
Although much is yet to be understood about fibromyalgia, research is uncovering the relationship between this condition and the immune system. This, in turn, is opening new treatment opportunities and pathways to explore.
Does Fibromyalgia Weaken The Immune System?
When the immune system experiences severe trauma, or it is called to respond to injury or infection (i.e.: Hepatitis C), it can start to malfunction. A malfunctioning immune system may produce autoantibodies that lead to autoimmune diseases, or it can become overactive and cause an increase in the activity levels of pain-sensing nerves.
These consequences can lead to the development of autoimmune diseases and chronic pain conditions like fibromyalgia. However, the opposite is also true: having fibromyalgia can lead to a weaker immune system.
Studies have shown that patients with fibromyalgia have high counts of pro-inflammatory cytokines (immune cells), which cause sustained inflammation. In turn, chronic inflammation can disrupt the functioning of the immune system and lead to autoimmune diseases and allergies.
In the long term, widespread inflammation can also lead to a cascade of complications. Firstly, it can damage healthy tissues, including cartilage and myelin, which is the nerves’ protective sheath. What’s more, when the immune system is constantly involved in the inflammatory response, it may not be able to correctly fight off harmful bacteria and viruses.
Lastly, ongoing inflammation can interfere with some of the body’s essential functioning, including digestion and sleep. A lack of appetite or sleep disturbances can further weaken the immune system and facilitate the development of illnesses.
2020 studies also show that fibromyalgia can be considered a low-cortisol state. Lower cortisol concentrations are associated with higher pain intensity, which is a symptom of fibromyalgia. Cortisol is a hormone responsible for regulating the stress response and the levels of estrogen in the body.
Low levels of cortisol cause estrogen levels to drop, which is associated with higher levels of progestin, a hormone that inhibits immune functions.
Over time, hormone fluctuations and chronic inflammation can compromise the immune system and make the development of other diseases and health conditions more likely.
The Challenges Of Diagnosing Fibromyalgia As An Autoimmune Disease
The symptoms of fibromyalgia are not immediately outwardly visible. Because of this, for many years, the very existence of this condition remained controversial. But, even more problematic is the fact that, due to the “invisible” nature of fibromyalgia, little research was conducted before the 1980s on the symptoms, causes, and outlook of fibromyalgia.
As a result, today, fibromyalgia remains challenging to diagnose and manage. And, given that the nature of this disease isn’t fully understood, no definitive treatments exist yet. Below, we’ll look into the challenges of diagnosing fibromyalgia as an autoimmune disease.
Difficulty In Identifying Common Symptoms And Causes
One of the main reasons why fibromyalgia remains hard to diagnose is that it is difficult for healthcare providers to identify the symptoms and causes of this condition.
Although the body of research around the causes of fibromyalgia has been growing since the 1970s, many patients today are forced to treat a condition with no identifiable cause. As seen above, current hypotheses outline how fibromyalgia may be caused by abnormalities in the functioning of the immune system, or by an interference with how the brain processes pain signals.
In patients who are at greater risk of suffering from this condition, fibromyalgia tends to start after other health events, like trauma, injury, illness, or mental health problems (i.e.: depressive episodes).
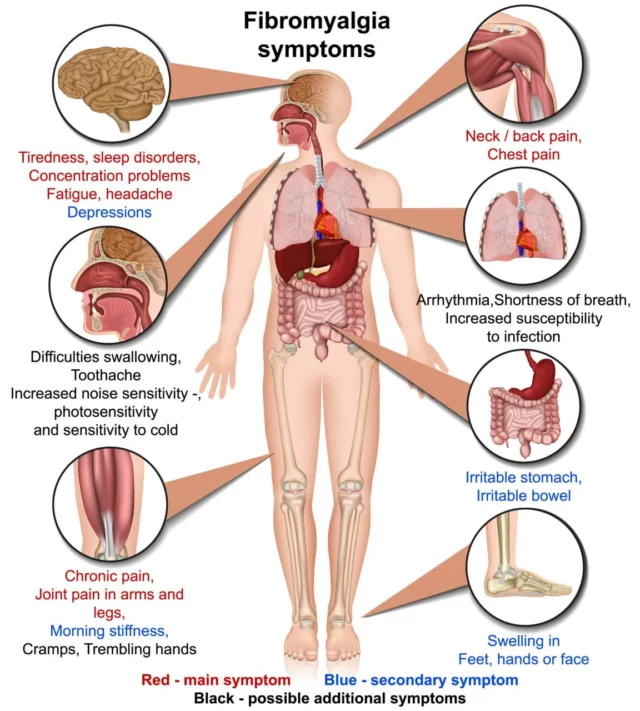
The symptoms of fibromyalgia are just as difficult to identify as its causes. Patients often experience widespread musculoskeletal pain, stiffness, fatigue, tiredness, anxiety, problems with memory, and headaches. Not only do these symptoms overlap with conditions like chronic fatigue syndrome, but they are also similar to other autoimmune diseases like rheumatoid arthritis.
A Lack Of Understanding Of Its Link To Autoimmunity
Besides the difficulty in identifying the symptoms of fibromyalgia, this condition remains challenging to diagnose as an autoimmune disease because it is not easily classified. According to the International Classification of Diseases (ICD-11), fibromyalgia is classified as a “chronic widespread pain” condition.
Nonetheless, a 2018 review shows that, even though fibromyalgia causes pain, it is more than just a pain condition or a somatic symptom disorder (a mental health condition that causes distress because of physical symptoms).
The picture is made more complicated by the fact that only recently the body of research has started to point towards fibromyalgia as an immune system disorder rather than a nerve condition. More research is needed to classify fibromyalgia as an autoimmune disease and facilitate its diagnosis.
Diagnostic Criteria For Fibromyalgia Is Not Well Defined
Diagnosing fibromyalgia is challenging due to the lack of reliable diagnostic procedures. Additionally, the symptoms of this condition can vary significantly from one person to another.
The first attempt to outline the diagnostic criteria for fibromyalgia took place in 1990 when the American College of Rheumatology determined 18 spots in the body that can be painful in people with fibromyalgia. If at the time of appointment, a patient experienced pain in at least 11 of these 18 “tender points”, they were diagnosed with this condition.
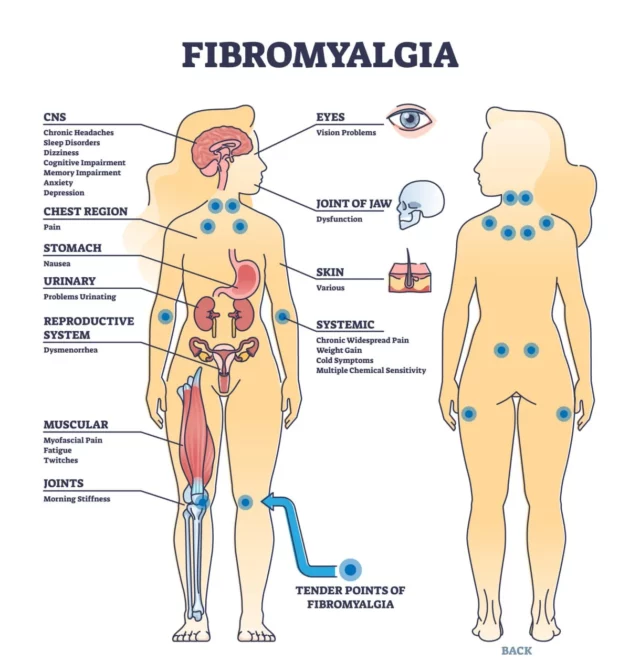
However, since this first attempt, the scientific community agreed that the pain caused by fibromyalgia changes in location and intensity constantly. So, basing a diagnosis on a set of static points was not an efficient strategy. To increase accuracy, the American College of Rheumatology upgraded the diagnostic criteria for fibromyalgia in 2010.
Today, diagnosing fibromyalgia involves a physical examination, blood tests, and a review of the patient’s symptoms. Your doctor may also prescribe a thyroid function assessment, checks for celiac diseases, tests to determine nutritional deficiencies, and a Rheumatoid Factor (RF) test to determine whether you may be at risk of this autoimmune disease.
Although these new diagnostic criteria help, most cases of fibromyalgia are diagnosed through exclusion.
Conventional Treatment Options For Fibromyalgia
Currently, there is no definitive cure for fibromyalgia. Most lines of treatment aim to reduce the symptoms of this condition and help people manage their pain to maintain a normal daily life.
If more research confirms the autoimmune nature of fibromyalgia, patients may start to take advantage of therapies to retrain and strengthen the immune system. However, for now, fibromyalgia is often treated through pharmacological therapies, alternative medicine practices, physical and occupational therapy, and stress management strategies.
Let’s look at how these approaches work below.
Lifestyle Changes
Positive lifestyle changes can go a long way to help you manage your fibromyalgia pain. Some steps to take include:
- Education: A 2021 study shows that the more a patient is educated about fibromyalgia and treatment options, the better he or she can cope with the symptoms. Education can also help you keep up with innovations and research updates.
- Improved sleep quality: The increased sensitivity to pain and distress caused by fibromyalgia cause sleep disruptions in over 95% of people with this condition. A lack of sleep translates into a decrease in pain threshold, increased daytime fatigue, higher levels of stress, and sustained inflammation.
- Staying active: Regular physical activity can help you increase your muscle strength, flexibility, and endurance. Aside from helping you build the foundations of overall health, regular exercise can help you remain independent in your daily life and trigger the release of endorphins, which are the body’s natural painkillers.
Medications
Pharmacological therapies are often the first line of treatment prescribed to patients with fibromyalgia. Common medications include:
- NSAIDs: Non-steroidal anti-inflammatory drugs are a class of drugs prescribed to manage to ease pain and inflammation. These drugs are often available over-the-counter, and they may be effective in the short term to reduce pain during a flare-up.
- Anti-seizure drugs: Antiepileptics are a class of drugs that modulate the normal pain signaling between the nerves and the brain. This helps manage an overactive transmission of pain and reduces pain sensitivity in people with fibromyalgia.
- Antidepressants and muscle relaxants: Antidepressants work by increasing the activity of neurotransmitters in the spinal cord responsible for reducing pain signals. Antidepressants also help promote feelings of relaxation, induce sleep, and help with depression.
Although these medications may help in the short term, it is important to note that they come with severe side effects, including fatigue, mood swings, increased risk of heart disease and stroke, gastrointestinal ulcers, and addiction.
Physical And Occupational Therapies
Some physical and occupational therapies can provide relief from fibromyalgia pain and offer guidelines to remain independent in your daily life despite your diagnosis. Some of these therapies include:
- Occupational therapy: An occupational therapist will be able to help you adjust your lifestyle to reduce fibromyalgia pain while keeping up with your work and hobbies.
- Physical therapy: Physical therapists will design exercise programs to boost your strength and flexibility. Recommended activities include yoga and aquatic exercises.
- Massage and acupuncture: Massage therapy and acupuncture can relieve muscle tension, stimulate the circulation of blood and oxygen, and trigger the release of feel-good hormones like endorphins. The combination of these actions can relieve pain and promote a sense of well-being.
- Stress-management techniques: Stress management techniques and mind-body exercises can relieve tension, boost your overall mental health, and increase your ability to cope with painful sensations. Some activities that may be beneficial for fibromyalgia pain include meditation, body scans, and biofeedback. A 2018 study also shows that breathing exercises “produced relevant benefits on pain threshold tolerance”.
Although these therapies may help you improve your mental, physical, and emotional well-being, it is important to note that your psychological health will impact your perception of pain and the progression of the disease. So, if you are experiencing fibromyalgia alongside depression or anxiety, a mental health professional should be your first port of call.
reference<https://neuragenex.com/is-fibromyalgia-an-autoimmune-disease/