The mitochondria have been featured more in and more post-infectious disease research. Health Rising’s first two overviews of recent mitochondrial findings featured long COVID and chronic fatigue syndrome (ME/CFS). Now we turn to fibromyalgia.
Dysfunctional mitochondria can cause pain as well.
The GIST
- Health Rising’s first two overviews of recent mitochondrial findings featured long COVID and chronic fatigue syndrome (ME/CFS). Now we turn to fibromyalgia.
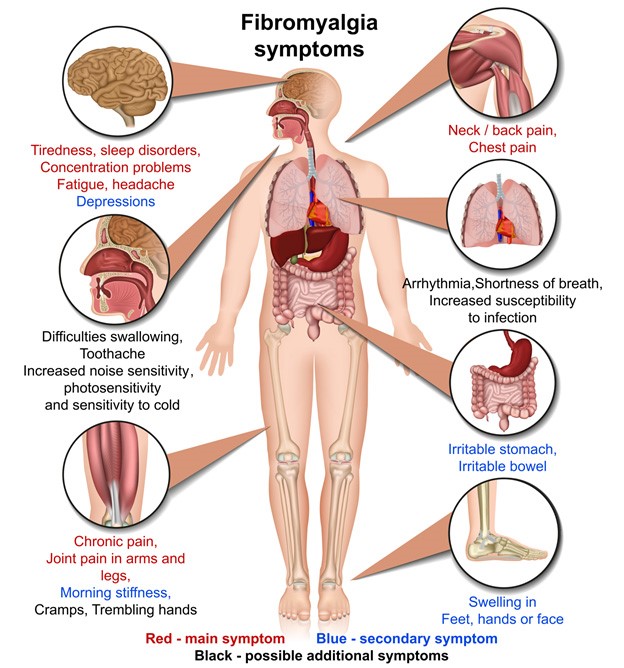
- We usually associate the mitochondria with extreme fatigue, exercise intolerance, and post-exertional malaise, but damaged mitochondria can also produce pain.
- With four studies published in the last year, the mitochondrial field in FM is going through a little boomlet.
- The first study – out of Italy – used the Seahorse XF Cell Mito Stress Test to find the cells of people with FM had a difficult time responding to mitochondrial stress, and put out 20% less energy than the healthy control. People with more severe FM, though, had it much worse. An energy index found they were about 40% in the red compared to healthy controls.
- Next, a Turkish study examining microRNA that negatively impact the mitochondria hit paydirt when it found a microRNA associated with oxidative stress far more commonly found (p<.0010) in the FM patients. That finding suggested oxidative stress – a common mitochondrial inhibitor – was greatly increased.
- The next study provided a potential answer to that issue. An Italian study provided a potential therapy for the high oxidative stress (see Treatment Takeaways below) The researchers induced a fibromyalgia-like state by giving rats a drug called reserpine, which, among other things, increases oxidative stress and knocks out the mitochondria.
- The rats had trouble moving, demonstrated muscle atrophy, reduced mitochondrial enzyme activity, showed decreased activity of most of the complexes in the electron transport chain (complex I, complex III, complex IV), and increased oxidative stress and mitochondrial DNA fragmentation, etc.
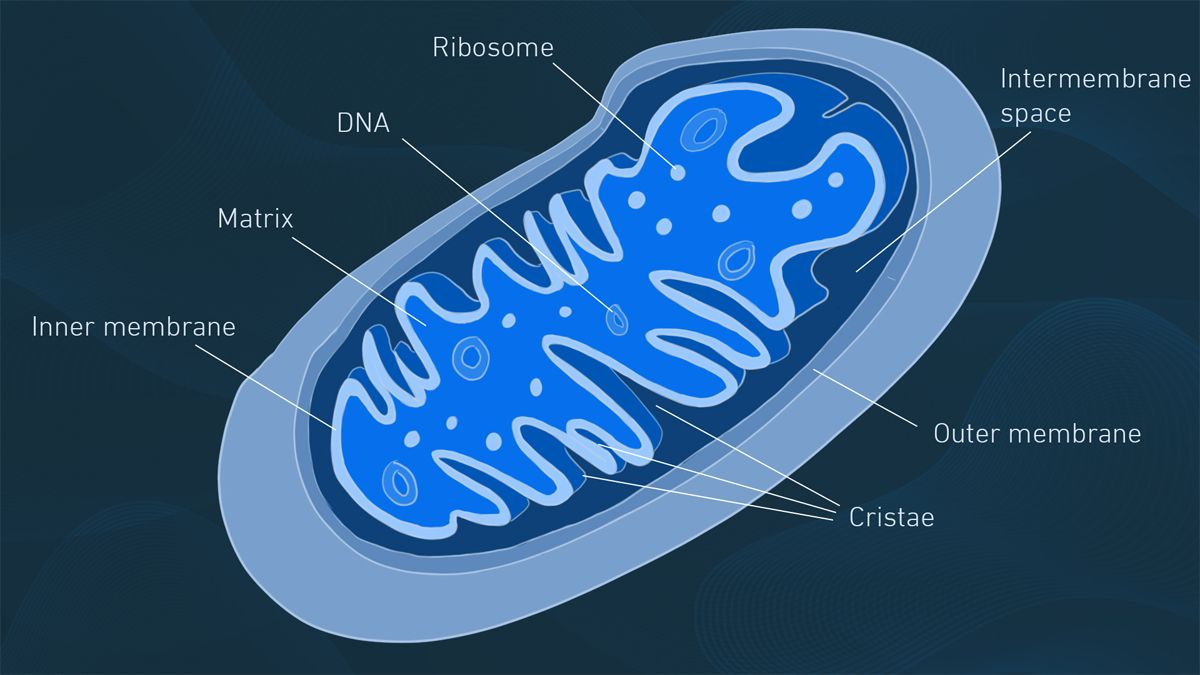
- The last study used an electron microscope to find reduced levels of the “cristae” or folds in FM patient’s mitochondria – where ATP production takes place. The authors proposed that the highly reduced ;levels of cristae found resulted from the mitochondria essentially turning itself off and putting the cells in a state of hibernation – much like Naviaux has proposed with ME/CFS.
- They suggested that the mitochondrial dysfunction in FM may impact a broad array of symptoms and tissues including the muscles, nerves, and gut and called the reduction in mitochondrial cristae a “rare and noteworthy’ objective finding.
- Taking the recent ME/CFS, fibromyalgia and long COVID studies together, the last year or so of mitochondrial suggests that a hypometabolic state akin to hibernation exists that may have been triggered a stressor such as an infection which first induced a hypermetabolic state which then essentially burnt out the mitochondria. High levels of oxidative stress are a likely culprit.
- A small but perhaps telling Stanford study found that stimulating the T-cells of ME/CFS patients overloaded their mitochondria, causing increased levels of T-cell death. Indeed energy production has been linked to poor performance of both T and B cells in ME/CFS.
Because we associate the mitochondria with extreme fatigue, exercise intolerance, and post-exertional malaise, we think of ME/CFS as the mitochondrial disease, not FM. The mitochondria do more than generate energy, though. Damaged mitochondria can also produce pain. Most people with heritable mitochondrial diseases suffer from chronic pain. Mitochondrial dysregulation appears to play a role in the transition from acute to chronic pain, and the introduction of healthy mitochondria into the sensory nerves at the dorsal root ganglia appears to resolve inflammatory pain.
Fibromyalgia, then, brings an interesting twist to the mitochondrial saga in the ME/CFS/FM/long-COVID disease space: mitochondrial problems in FM could be contributing to both exercise and pain and sensory problems.
With four studies published in the last year, the mitochondrial field in FM is going through a little boomlet.
Reduced Energy Production
The latest, “Mitochondrial function in patients affected with fibromyalgia syndrome is impaired and correlates with disease severity“, came out of Italy.
The Italians used the Seahorse XF Cell Mito Stress Test which measures the oxygen consumption (i.e. aerobic energy production) of cells at baseline, during stress, and during mitochondrial enhancement. Researchers can determine such things as mitochondrial respiration, reserve capacity, and the proton leak.
The peripheral blood mononuclear cells of fifty people with FM and 20 healthy age and sex-matched controls were assessed.
The study found a 27% reduction in maximal respiration; the ability of the mitochondria to produce maximal amounts of energy. A reduction in spare respiratory capacity indicated that the FM patients’ mitochondria lacked the reserves to respond to stress that the healthy controls had. An overall assessment of mitochondrial functioning called the bioenergetic health index (BHI) found that the FM patients were about 20% in the red compared to the healthy controls.
Things only got worse with the more severe FM patients. With BHI and spare reserve capacity reduced by another 20%, the more severe patients were looking at a 40-50% functional hit to their mitochondria.
Correlating symptoms (Fibromyalgia Severity Score (FSS)) with the mitochondrial findings, however, produced only a low to moderate finding; i.e. the mitochondrial findings didn’t seem to be contributing that much to fibromyalgia symptoms measured by that test.
Mitochondria on Fire?

One miRNA was greatly increased in the FM patients.
Next, a Turkish study, “Mitochondria miRNAs and Fibromyalgia: New Biomarker Candidates“, isolated and then assessed the gene expression of the mitochondria via microRNAs (miRNAs) in 35 FM patients and healthy controls.
Gene expression studies assess the “state” of the cell, tissue, or in this case, organelle. They tell us what genes are turned on or off, the health of the cell, if it is stressed, and what it’s responding to, etc.
Genes express themselves through the strands of RNA that cells produce. By determining which RNAs get expressed, miRNAs regulate the gene expression of cells.
This Turkish team must have been pretty confident in their idea that the mitochondria are having problems in FM because they honed in on just three mitochondrial miRNAs (mitomiRs): mitomiR-145-5p, mitomiR-223-3p, and mitomiR-23a-3p.
They hit paydirt: the mitomiR-145-5p miRNA stuck out like a sore thumb and was vastly more commonly found (p<.0010) in the FM patients. The miRNA finding suggested a common theme was present – oxidative stress was out of control.
That fits with several recent findings suggesting that damaged mitochondria produce high levels of oxidative stress, which, in turn, damages the mitochondria further, and leads to immune cell exhaustion in ME/CFS.
Health Rising’s End of the Year Fundraising Drive
If getting the latest news on cutting-edge research and treatments in ME/CFS, fibromyalgia, long COVID, and related diseases supports you, please support Health Rising in it’s end of the year fundraising drive. We are entirely community supported.
Paypal, checks, Amazon gift cards, and bitcoin work for us.
Use the widget on the right hand side to donate via Paypal or click here. To find out more, click here. Thanks!
Boswellia to the Rescue?
The next study provided a potential answer to that issue. Another Italian study, “Impaired mitochondrial quality control in fibromyalgia: Mechanisms involved in skeletal muscle alteration“, induced a fibromyalgia-like state by giving rats reserpine. Reserpine is a nasty chemical that does things like reduce serotonin, norepinephrine, and dopamine levels, increase oxidative stress, hammer mitochondrial production, and enhance inflammation… In other words, it’s perfect!
The authors were primarily interested in the rats’ muscles and central nervous system. FM muscle studies found evidence of muscle damage including ragged red fibers, irregularities in mitochondrial structure, mitochondrial myopathies, and deficiencies in the last complex of the electron transport chain.
Reserpine hit the muscles and the mitochondria hard. The rats had trouble moving, demonstrated muscle atrophy, reduced mitochondrial enzyme activity, showed decreased activity of most of the complexes in the electron transport chain (complex I, complex III, complex IV), and demonstrated increased oxidative stress and mitochondrial DNA fragmentation, etc.
An accompanying spinal and brain study found the reserpines’ activation of glial cells in two key pain regions (dorsal horn of the spinal cord / prefrontal cortex) probably caused central sensitization; the amplification of the pain-producing pathways in the brain.
The FM rats soon had a reprieve, though. Treating them orally with Boswellia gum extract reduced their oxidative stress, decreased their mitochondrial problems, restored mitochondrial enzyme production, increased mitochondrial production, and restored the functioning of one of the complexes.
Increased myogenin production suggested the rats were also now adapting to exercise well. Increased levels of PGC-1α and other factors relating to the production of mitochondria suggested that “mitochondrial biogenesis” – the production of more and more mitochondria, a key part of muscle development – was proceeding smoothly.

Boswellia extract proved to have high mitochondria rejuvenating powers. (The Boswellia tree).
Boswellia extract
Treatment Takeaways
- Boswellia extract reduced the FM rats oxidative stress, decreased their mitochondrial problems, restored mitochondrial enzyme production, increased mitochondrial production, and restored the functioning of one of the complexes.
- Boswellia has been used to treat inflammatory conditions like rheumatoid arthritis, asthma and inflammatory bowel disease. Instead of directly enhancing mitochondrial functioning, Boswellia protects the mitochondrial enzymes and the electron transport chain from the ravages of oxidative stress.
- Interestingly, when asked about Boswellia and the mitochondria, AI ChatGPT stated that Boswellia’s ability to enhance ATP production is “especially relevant in diseases associated with mitochondrial dysfunction, such as chronic fatigue syndrome and fibromyalgia, where fcellular energy demand often exceeds supply.” (!
- Re