- Periods
- Pains and aches
- IBS and PBS
- Fatigue and depression
- Other symptoms
- When to see a doctor
- Treatment
Fibromyalgia in women
Fibromyalgia is a chronic condition that causes fatigue, widespread pain, and tenderness throughout the body. The condition affects both sexes, although women are far more likely to develop fibromyalgia. Between 80 and 90 percent of people who get a diagnosis are women, according to the National Institutes of HealthTrusted Source.
Sometimes men receive a misdiagnosis because they may describe fibromyalgia symptoms differently. Women often report higher pain intensity than men. The reasons behind this may be related to hormones, immune system differences, or genes.
Still, researchers aren’t sure why women have a higher risk for developing fibromyalgia than men. The only way to test for it is to rule out other possible conditions.
Read on to learn how different fibromyalgia symptoms can feel for women.
Menstrual period cramps can be mild or painful, depending on the woman. In a report by the National Fibromyalgia Association, women with the condition have more painful periods than usual. Sometimes the pain fluctuates with their menstrual cycle.
Most women with fibromyalgia are also between the ages of 40 to 55 years old. Fibromyalgia symptoms may feel worse in women who are postmenopausal or are experiencing menopause.
Menopause with fibromyalgia may increase feelings of:
- crankiness
- soreness
- achiness
- anxiety
Your body produces 40 percent less estrogen after menopause. Estrogen is a huge player in controlling serotonin, which controls pain and mood. Some fibromyalgia symptoms can mirror symptoms of perimenopause, or “around menopause.” These symptoms include:
- pain
- tenderness
- lack of quality sleep
- trouble with memory or thinking through processes
- depression
Some women with fibromyalgia also have endometriosis. In this condition, cells similar to those that line the uterus grow in other parts of the pelvis. Fibromyalgia can also increase the discomfort that endometriosis causes. Talk to your doctor if these symptoms don’t go away after menopause.
Home remedies to soothe your menstrual cramps »
Amplified fibromyalgia pain is often described as a deep or dull ache that starts in the muscles and radiates to other parts of the body. Some people also have a pins and needles sensation.
For a fibromyalgia diagnosis, the pain must affect all parts of your body, on both sides including the upper and lower parts. The pain may come and go. It can be worse on some days than on others. This may make it hard to plan for daily activities.
What’s interesting is that men and women experience fibromyalgia pain differently. Both report experiencing an intense level of pain at some point in time. But overall men tend to report a lower pain intensity than women. Women experience more “all-over hurting” and longer durations of pain. Fibromyalgia pain is often stronger in women because estrogen decreases pain tolerance.
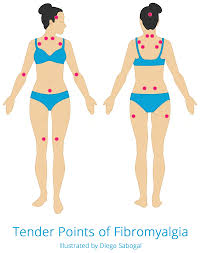
Tender points
In addition to widespread pain, fibromyalgia causes tender points. These are specific areas around the body, usually near your joints that hurt when they are pressed on or touched. Researchers have identified 18 possible tender points. On average, women report at least two more tender points than men. These tender points are also more sensitive in women. You may experience pain in some or all of these places:
- back of the head
- area between the shoulders
- front of the neck
- top of the chest
- outside of the elbows
- top and sides of the hips
- insides of the knees
Tender points can also appear around the pelvic area. Pain that’s ongoing and lasts for more than six months is called chronic pelvic pain and dysfunction (CPPD). These aches can start in the back and run down the thighs.
Fibromyalgia can make worse other issues related to CPPD, such as irritable bowel syndrome (IBS) and bladder problems. Research shows that people with fibromyalgia and IBS also have a higher chance of developing interstitial cystitis, or painful bladder syndrome (PBS). Roughly 32 percent of people who have IBS also have PBS. Studies show that IBS is also more common in women. Roughly 12 to 24 percent of women have it, while just 5 to 9 percent of men have IBS.
Both PBS and IBS can cause:
- pain or cramps in the lower abdomen
- pain during intercourse
- pain during urination
- pressure on the bladder
- increased need to pee, all times of the day
Research suggests that both PBS and IBS have similar causes to fibromyalgia, although the exact relationship is unknown.
more
A study, published in the Oxford University Press, looked at the occurrences of depression in men and women who have fibromyalgia. Researchers found that women who have the condition reported significantly higher levels of depression than men.
Other conditions that often occur alongside fibromyalgia can keep you awake at night. These include restless legs syndrome and sleep apnea. A lack of sleep can contribute to feelings of fatigue and depression. You may feel tired and have trouble concentrating during the day, even with a full night’s rest. An inappropriate amount of sleep can also increase your sensitivity to pain.
other symptom
Other common symptoms of fibromyalgia include:
- sensitivity to temperature drops, loud noises, and bright lights
- trouble remembering and concentrating, also called fibro fog
- headaches, including migraines that cause nausea and vomiting
- restless legs syndrome, a creepy, crawly feeling in the legs that wakes you from sleep
- jaw pain
when to see a doctor
Talk to your doctor if these symptoms interfere with your well-being or accompany other symptoms of fibromyalgia. There’s no single exam to diagnose fibromyalgia. The symptoms can be similar to other conditions such as rheumatoid arthritis (RA). But unlike RA, fibromyalgia doesn’t cause inflammation.
This is why your doctor will do a physical examination and order multiple tests to rule out other conditions.
How is fibromyalgia diagnosed? »
Fibromyalgia isn’t life-threatening, but it can affect your quality of life. Early treatment can slow the progression of fibromyalgia.
0 seconds of 0 secondsVolume 0%
treetment
There’s no cure for fibromyalgia, but treatment is available. You can still manage the pain and live a healthy, active life.
Some people are able to manage pain with over-the-counter (OTC) pain relievers, such as acetaminophen, ibuprofen, and naproxen sodium. Your doctor may prescribe specific medications to reduce pain and fatigue, if OTC drugs don’t work.
These drugs include:
- duloxetine (Cymbalta)
- gabapentin (Neurontin, Gralise)
- pregabalin (Lyrica)
A study from 1992 study showed that people who took malic acid and magnesium reported significant improvement in muscle pain within 48 hours. The pain came also back in people who took a placebo pill after 48 hours. But no recent studies have been done on this combination for fibromyalgia treatment.