While no one knows what exactly causes fibromyalgia, doctors do know a few things about the condition: The widespread chronic pain disorder seems to involve the nervous system; affects 2 to 4 percent of Americans, mostly women; and commonly occurs in people who have other types of musculoskeletal pain, such as different kinds of arthritis.
But unlike many musculoskeletal conditions, fibromyalgia isn’t an inflammatory or autoimmune disease — when your immune system, which normally protects your body from infection, turns against itself and attacks your own cells and tissues. That can produce chronic inflammation that can eventually damage your body. Fibromyalgia is also not a joint or muscle disorder caused by physical injury.
Instead, experts think that fibromyalgia is neurological in nature.
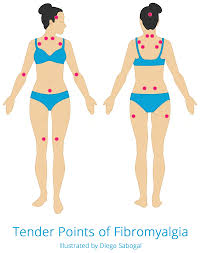
“Fibromyalgia is a disorder in which the sensitivity to pain has been turned up in the brain,” says J. Michelle Kahlenberg, MD, PhD, an associate professor in the division of rheumatology at the University of Michigan Medical School in Ann Arbor. “Chemical transmitters in the brain have gotten reprogrammed so that they are firing pain signals with very minimal stimuli. A squeeze of the arm, a shake of the hand, a touch on the shoulder — all of those things can be very painful for people with fibromyalgia.
which include widespread pain, sensitivity to touch, sleep issues and fatigue, brain fog, gastrointestinal distress (bloating and diarrhea), and mental health issues like depression and anxiety — propel you into the doctor’s office, your provider must first rule out other conditions that could be responsible for your fibro symptoms.
“That’s why fibromyalgia can be underdiagnosed, because we have to look for everything else first. On the other hand, fibromyalgia can also be overdiagnosed, because there’s no specific blood work or imaging tests that we can do to diagnose it,” Dr. Kahlenberg explains.
medications to slow its progress as well as steroids, such as prednisone, to reduce nerve inflammation during MS flares. People with MS are also helped by physical therapy and medications to reduce fatigue.
Unlike MS, fibromyalgia isn’t a progressive disease and so it won’t damage your muscles or organs. But there is a connection between MS and fibromyalgia. “Any time patients have an autoimmune disease, there is a chance that they could develop fibromyalgia because of the stress and the chronic pain that comes from the autoimmune disease,” Dr. Kahlenberg explains. “Those things can reprogram the central nervous system, and crank up that pain volume receptor, so that even if we get the inflammation in their joints and muscles under control, the volume receptor can remain high.”
In other words, if you have an MS diagnosis, there’s a chance you can also have fibro along with it.
3. Rheumatoid Arthritis
Like many of the conditions mixed up with fibro, rheumatoid arthritis is an autoimmune disorder. It involves inflammation in the lining of your joints, called the synovium. It typically starts in the small joints in the hands and feet, though the body-wide inflammation in RA can also affect other parts of your body, including the skin, eyes, heart, lungs, and more.
And like patients with fibromyalgia, people with RA often have fatigue, weakness, and constant pain. And though the pain is in the joints, it can be tough to tell where specifically where it’s coming from when you ache all over.
But with RA you will have stiff joints — and that’s a key difference from fibromyalgia, according to Dr. Morris. “Patients with inflammatory diseases often are stiff for hours, while fibromyalgia patients usually can loosen up with 30 to 40 minutes,” he notes. Plus, there is swelling in the joints with RA, which isn’t the case for those with fibromyalgia, whose pain symptoms are more in the muscles, he adds.
diabetes, which means their bodies can’t regulate blood sugar (glucose). Type 2 diabetes can produce general achiness and fatigue that mimic fibromyalgia, he says. But unlike fibro, the condition can lead to serious complications, including strokes, glaucoma, and heart disease, which is why it’s super-important to catch and treat it. Diabetes is easily diagnosed based on the levels of sugar in your blood or urine.
8. Anemia
Feeling tired is also a hallmark of anemia, which occurs when your body does not produce enough healthy red blood cells to carry the oxygen you need. If you’re anemic, you’ll also be weak and have headaches, just as you would with fibromyalgia, though you may not have pain or tingling in your muscles. The most common form of anemia is due to a lack of iron, but inflammation (say, from RA) can also cause anemia as can blood disorders and cancers. That’s why providers check red blood counts as they narrow their diagnosis.
9. Chronic Fatigue Syndrome
Think of chronic fatigue syndrome and fibromyalgia as flip sides of almost identical chronic conditions. Patients with CFS have many similar symptoms as those with fibro — brain fog, constant exhaustion, headaches, and poor sleep. And like fibromyalgia, women are much more likely to have CFS than men.
But there are differences between them. People with chronic fatigue have enlarged lymph nodes and sometimes a sore throat. And most importantly, the fatigue is more overpowering than the pain (the reverse is true in fibromyalgia).
Doctors aren’t exactly sure what causes chronic fatigue syndrome, though some think its origins could be viral — from the flu, say, or the virus that causes mononucleosis. But your provider will arrive at a diagnosis of CFS in a similar way to that of fibromyalgia, by excluding other conditions through careful sleuthing and tests.
Treatment can be tricky too. Sometimes even the gentlest workouts can make CFS symptoms worse (while they can be beneficial for patients with fibro, especially meditative exercise like tai chi, says Dr. Kahlenberg). Cognitive behavior therapy can help manage chronic pain, as can antidepressants, since CFS patients also have depression (understandably).