Fibromyalgia is a complex and multisystem disorder known for causing widespread pain, fatigue, and cognitive dysfunction. However, many people with fibromyalgia also experience chronic postnasal drip—a condition in which mucus from the nasal passages drips down the back of the throat, causing irritation, coughing, and congestion.
While postnasal drip is often linked to allergies, sinus infections, or environmental triggers, fibromyalgia patients may experience persistent nasal and throat issues without an obvious cause. This raises the question: Is postnasal drip a symptom of fibromyalgia, or is there an underlying link between the two conditions?
In this article, we will explore the connection between fibromyalgia and postnasal drip, including potential causes, symptoms, and effective management strategies.
about:blank
1. What Is Postnasal Drip?
Postnasal drip occurs when the mucous glands in the nose and throat produce excessive mucus, which accumulates in the back of the throat instead of being naturally cleared.
Common symptoms include:
about:blank
✔ A constant need to clear the throat
✔ Persistent cough, especially at night
✔ A sensation of mucus stuck in the throat
✔ Hoarseness or sore throat
✔ Nasal congestion or stuffiness
Postnasal drip is often associated with conditions such as sinus infections, allergies, colds, or acid reflux. However, many fibromyalgia patients experience it without an obvious trigger, suggesting a potential link between fibromyalgia and chronic mucus production.
2. The Link Between Fibromyalgia and Postnasal Drip
Although fibromyalgia is primarily a neurological disorder that affects pain perception, it can also impact the immune system, autonomic nervous system, and mucus production.
about:blank
Here are some possible connections between fibromyalgia and postnasal drip:
1. Autonomic Nervous System Dysfunction (Dysautonomia)
✔ Fibromyalgia is linked to autonomic nervous system dysfunction, which affects involuntary body functions like mucus production, heart rate, and digestion.
✔ Overactive mucous glands in the nasal passages may result in excessive mucus, leading to postnasal drip.
2. Chronic Inflammation and Immune System Dysfunction
✔ Many fibromyalgia patients experience chronic low-grade inflammation, which may affect the sinuses, throat, and nasal passages.
✔ Overactive immune responses could trigger excessive mucus production as a defense mechanism.
about:blank
3. Increased Sensitivity to Environmental Triggers
✔ People with fibromyalgia often have heightened sensitivities to allergens, chemicals, and weather changes.
✔ Even mild irritants (dust, perfumes, pollen) can cause sinus inflammation and excessive mucus buildup.
4. Acid Reflux (Silent GERD) in Fibromyalgia
✔ Many fibromyalgia patients suffer from gastroesophageal reflux disease (GERD), which can cause stomach acid to irritate the throat and sinuses.
✔ This irritation can stimulate mucus production, worsening postnasal drip symptoms.
5. Medication Side Effects
✔ Fibromyalgia treatments, including antidepressants, muscle relaxants, and pain medications, may cause dry mouth and nasal irritation.
✔ In response, the body may produce extra mucus to compensate, leading to postnasal drip.
about:blank
6. Sleep Issues and Nighttime Mucus Accumulation
✔ Fibromyalgia patients often struggle with poor sleep quality and nasal congestion at night.
✔ Lying down for long periods can allow mucus to accumulate in the throat, causing morning postnasal drip and throat irritation.
3. Symptoms of Postnasal Drip in Fibromyalgia
Postnasal drip symptoms can be mild or severe and may fluctuate based on weather, diet, stress, and environmental triggers.
about:blank
Common symptoms include:
✔ Constant throat clearing and irritation
✔ Persistent cough, especially worse at night
✔ Sensation of mucus stuck in the throat
✔ Hoarseness or voice changes
✔ Nasal congestion and sinus pressure
✔ Increased mucus production after eating certain foods
For fibromyalgia patients, these symptoms may persist even without allergies or infections, making them more frustrating and difficult to treat.
about:blank
4. How to Manage Postnasal Drip in Fibromyalgia
Although postnasal drip can’t always be cured, there are several ways to reduce symptoms and improve nasal health.
1. Stay Hydrated
✔ Drink plenty of water throughout the day to thin mucus and prevent throat irritation.
✔ Avoid excess caffeine and alcohol, as they can lead to dehydration and thicker mucus.
2. Use a Saline Nasal Spray or Neti Pot
✔ Rinsing the sinuses with a saline spray or a neti pot can help clear excess mucus and reduce nasal irritation.
✔ This is especially helpful for fibromyalgia patients sensitive to allergens or dry air.
about:blank
3. Elevate Your Head While Sleeping
✔ Keeping your head slightly elevated prevents mucus from pooling in the throat.
✔ Try using a wedge pillow or adjustable bed to improve drainage
4. Avoid Mucus-Producing Foods
✔ Dairy products, fried foods, and processed sugars can thicken mucus and worsen postnasal drip.
✔ Stick to anti-inflammatory foods like fruits, vegetables, and lean proteins.
5. Try Steam Inhalation
✔ Inhaling steam moisturizes nasal passages and loosens mucus buildup.
✔ Add essential oils like eucalyptus or peppermint to a bowl of hot water and breathe in the steam for relief.
about:blank
6. Manage Acid Reflux (If Present)
✔ If you have silent acid reflux (GERD), avoid spicy, acidic, or greasy foods.
✔ Taking antacids or acid reducers before bedtime may help reduce postnasal drip symptoms.
7. Identify Medication Side Effects
✔ If postnasal drip worsens after starting a new medication, speak with your doctor about alternative options.
✔ Some antidepressants and pain medications may dry out the nasal passages, triggering rebound mucus production.
8. Reduce Environmental Triggers
✔ Use an air purifier to reduce airborne allergens and dust.
✔ Avoid strong perfumes, smoke, and chemical irritants that may increase nasal congestion.
about:blank
5. When to See a Doctor
If postnasal drip becomes chronic or is accompanied by severe sinus pain, difficulty breathing, or fever, seek medical attention.
You may need to see:
✔ An ENT specialist (Ear, Nose, and Throat doctor) to check for sinus issues or nasal inflammation.
✔ An allergist if symptoms worsen with seasonal changes or specific triggers.
✔ A gastroenterologist if acid reflux is contributing to excessive mucus production.
about:blank
6. Conclusion: Addressing Postnasal Drip in Fibromyalgia
Postnasal drip is an under-recognized but common issue in fibromyalgia patients. It may be linked to autonomic nervous system dysfunction, inflammation, allergies, or medication side effects.
By staying hydrated, clearing nasal passages, avoiding trigger foods, and managing acid reflux, fibromyalgia patients can reduce mucus buildup and improve throat comfort.
If postnasal drip symptoms persist despite home remedies, consulting a healthcare provider can help identify the underlying cause and determine the best treatment plan.
about:blank
Would you like personalized strategies to manage postnasal drip and fibromyalgia symptoms?
49 Fibromyalgia Symptoms – Anyone with muscle pain should read this
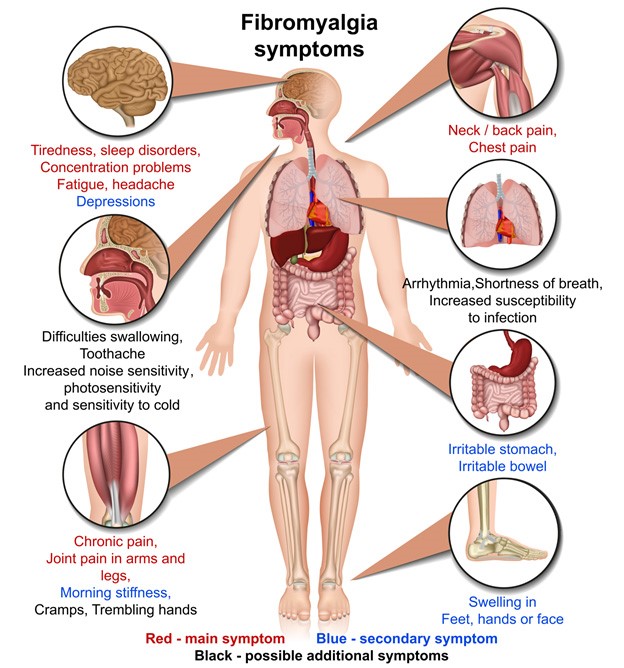
In America, between three and six million people, or one in every fifty, suffer from fibromyalgia, a syndrome characterized by debilitating pain throughout the body without any obvious cause. Although people often improve over time, it is often something they will have to face for life.
If you have chronic muscle pain, however, it does not necessarily mean that you have fibromyalgia. If you are concerned that you may have fibromyalgia, it is important to keep in mind that there are many other symptoms that accompany muscle pain. Take a look at the signs and symptoms below to get a better understanding.
about:blank
Symptoms of fibromyalgia
If you find that your muscles are sore on a constant basis without obvious external causes, consult this list of symptoms to help you determine if you could have fibromyalgia
All the symptoms are unlikely to match, but if most of them resonate with you, then bring your concerns to the doctor who will be able to rule out all other causes first.
about:blank
Muscles and
muscle tissues Spasm muscles
Morning stiffness
Swelling
Mild and intense pains that can move to different parts of the body
Soft and knotty breasts (fibrocystic breast, like an overlap)
Sleep problems
Tiredness
Grinding of teeth
even during sleep
Feeling Falling asleep (“Starts sleep”)
Difficulty sleeping / broken sleep, leaving you tired and apathetic every morning rather than refreshed.
Allergic and sinus disorders
Ringing ears Thick
mucus
Itchy ears and earaches
Nose drip and post nasal drip
Allergies, sensitivity to molds and yeasts
Shortness of breath
Stomach problems and digestion
Swelling, nausea, abdominal cramps and pelvic pain
Frequent urination (always need to pee, get up every night, often more than once)
IBS
Sensory Problems and Sensitivity
Sensitive to odors, light, noise, temperature, pressure and climate change.
Difficulty with night driving and seeing in poor lighting conditions
Cognitive difficulties
Poor coordination and balance
Directional difficulties and recognizing familiar environments
Exclude often, difficulty concentrating, short-term memory and differentiation between certain shades of color.
Burning or tingling in the upper limbs
Impaired language and difficulty speaking familiar words
Reproductive problems
Loss of libido
Impotence
PMS and other menstrual problems
Problems
cardiac Irregular heartbeat Problems with
valves
pain similar to a heart attack
hair, skin and nails
Nails or overprinted nails sagging under the
skin that bruises or scars easily or appears mottled
Hair Loss
Mental Health Symptoms
Anxiety, depression, panic attacks
Unexplained mood swings and irritability
Other symptoms
Family history
Unexplained weight gain or weight loss
Carbohydrates and chocolate cravings
Headaches and migraines
Visual changes
Sweating
Remember that all these signs and symptoms are not specific, which means that they can be caused by or indicate another condition, or they could be random and mean absolutely nothing. For example, just because PMS occur, from time to time they are moody, have cravings, or experience migraines, does not mean that you have fibromyalgia. Once again, talk to your doctor before jumping to any conclusion.
How is fibromyalgia diagnosed?
Unfortunately, fibromyalgia can be confused with other conditions, and there are no specific tests that can give one hundred percent certain diagnoses, making diagnosis difficult.
First of all, you must meet the specific criteria set by the American College of Rheumatology to receive a diagnosis of fibromyalgia.
about:blank
Widespread pain that has been present for at least 3 months in all four quadrants of the body
11 out of 18 painful points, with pain felt when palpated on those points
Negative results for any other disease on any of the diagnostic tests performed
Because there is no a test that can determine if someone has fibromyalgia, doctors use a combination of diagnostic tests to help rule