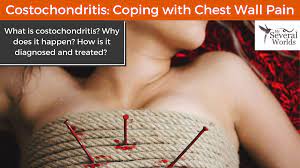
f you have fibromyalgia (FMS), chest pain may be one of your symptoms. A condition called costochondritis, which causes pain around the breastbone and rib cage, could be to blame. It is caused by inflammation in the cartilage that connects your ribs and sternum (breastbone). It’s believed to be common in people with FMS.1
Costochondritis is also called noncardiac chest pain or musculoskeletal chest pain. It does not involve the heart, but it is sometimes confused with heart palpitations. Because any other sources of pain can make your FMS symptoms worse, it’s crucial to treat costochondritis.2
Fibromyalgia chest pain can make you think you’re having heart problems, which is a scary thing. Even though costochondritis is common, you should get medical attention if you have unexplained chest pain.3 You don’t want to assume that it’s FMS-related and end up with permanent heart damage or worse.
This article discusses more about what causes costochondritis, how fibromyalgia chest pain is diagnosed, and how to treat it.
Causes of Costochondritis
Costochondritis is caused by inflammation of the cartilage that connects your ribs to your breastbone. Depending on how much inflammation there is, it can range from mildly annoying to intensely painful. People sometimes describe the pain as stabbing, aching, or burning.4
The causes of costochondritis aren’t clear, but they may include:
- Chest trauma, such as from a car accident
- Repetitive trauma or overuse
- Viral infections, especially upper respiratory infections
Some experts believe costochondritis and fibromyalgia are related. Regardless, because FMS amplifies pain, it can make costochondritis much more painful.
Costochondritis and Fibromyalgia: The Connection
Many people with FMS have symptoms very similar to costochondritis. In one study, non-specific chest pain is listed as the most common additional symptom in people who were hospitalized with FMS.5 Another lists FMS as a frequent cause of musculoskeletal chest pain.6
No one is exactly sure whether this is actually costochondritis or why it occurs with FMS. One hypothesis is that FMS involves inflammation of the fascia, which is a thin layer of connective tissue that runs all through your body.7 If that’s true, it may explain the connection between costochondritis and fibromyalgia.
The fibromyalgia tender points just beneath the collarbone may play a role as well. These pressure points are 18 spots on the body once used to diagnose fibromyalgia. If you feel localized pain when someone presses on a spot with enough force for their finger to turn white, it’s likely that the spot is a tender point.
Myofascial pain syndrome, which is common in people with FMS, also could be a cause of costochondritis.
Costochondritis is typically a minor injury, but it can take several weeks or months to resolve.8 If symptoms don’t clear up, it could be a sign that your chest pain is caused by fibromyalgia.
:max_bytes(150000):strip_icc():format(webp)/costochondritis-in-fibromyalgia-716178_FINAL-5c92ae8746e0fb0001ac1350.png)
Costochrondritis Symptoms
Pain in the chest wall and rib cage is the chief symptom of costochondritis. Generally, the pain will flare up when you:
- Exercise or do another physical activity
- Take a deep breath (this stretches the inflamed cartilage)
- Sneeze
- Cough
The pain can radiate to your shoulder and arms as well (another way the condition mimics a heart attack).
Sometimes the pain is accompanied by redness and/or swelling in the most painful areas. When that’s the case, it’s called Tietze’s syndrome.9
Diagnosing Fibromyalgia Chest Pain
Your healthcare provider can diagnose fibromyalgia chest pain by pressing on the area where the ribs and breastbone come together. If it’s tender and sore there, costochondritis is the most likely cause of pain. Healthcare providers generally will perform other tests to rule out heart problems and other causes of pain before diagnosing costochondritis and fibromyalgia.
Treating Fibromyalgia Chest Pain
You can treat costochondritis the way you’d treat any inflammation—ice and anti-inflammatory drugs, including Aleve (naproxen) and ibuprofen-based drugs such as Advil and Motrin.10
This treatment sometimes runs counter to FMS treatments, which can include other types of pain relievers and heat. If you have fibromyalgia chest pain, you might find yourself with an ice pack on your chest and a heating pad on your back at the same time.
Be sure to check with your healthcare provider or pharmacist about any possible interactions between anti-inflammatories and your other medications.
In addition, exercise may help improve fibromyalgia-related chest pain. The Centers for Disease Control and Prevention says that moving your body (it recommends at least 30 minutes of moderate physical activity five days a week) may help reduce pain and improve your mood.1112
Your healthcare provider may recommend other types of treatment as well, including physical therapy or acupuncture.
Outlook for Fibromyalgia Chest Pain
Fibromyalgia chest pain typically goes away in a few days or weeks, but can sometimes take months.13 While you’re waiting for it to go away, continue to take steps to help reduce symptoms. In most cases, this condition shouldn’t prevent you from doing daily activities.
If your chest pain is associated with fibromyalgia, it may not clear up as fast or at all. People with fibromyalgia can experience a lower quality of life, and this added source of pain may contribute to this.12 However, continuing with treatment such as medication, ice packs, and exercise can help to lift your mood by minimizing your symptoms.
A Word From Verywell
It’s bad enough to live with one source of chronic pain. The more you heap on, the more pain you’ll have and the more it can impact your life. Fortunately, fibromyalgia chest pain is fairly easy and inexpensive to treat, and managing it will keep it from exacerbating your FMS symptoms.
13 Sources
:max_bytes(150000):strip_icc():format(webp)/Adrienne-Dellwo-1000-749dc7aac3884bb1bf77744fafac64ef.jpg)
By Adrienne Dellwo
Adrienne Dellwo is an experienced journalist who was diagnosed with fibromyalgia and has written extensively on the topic.