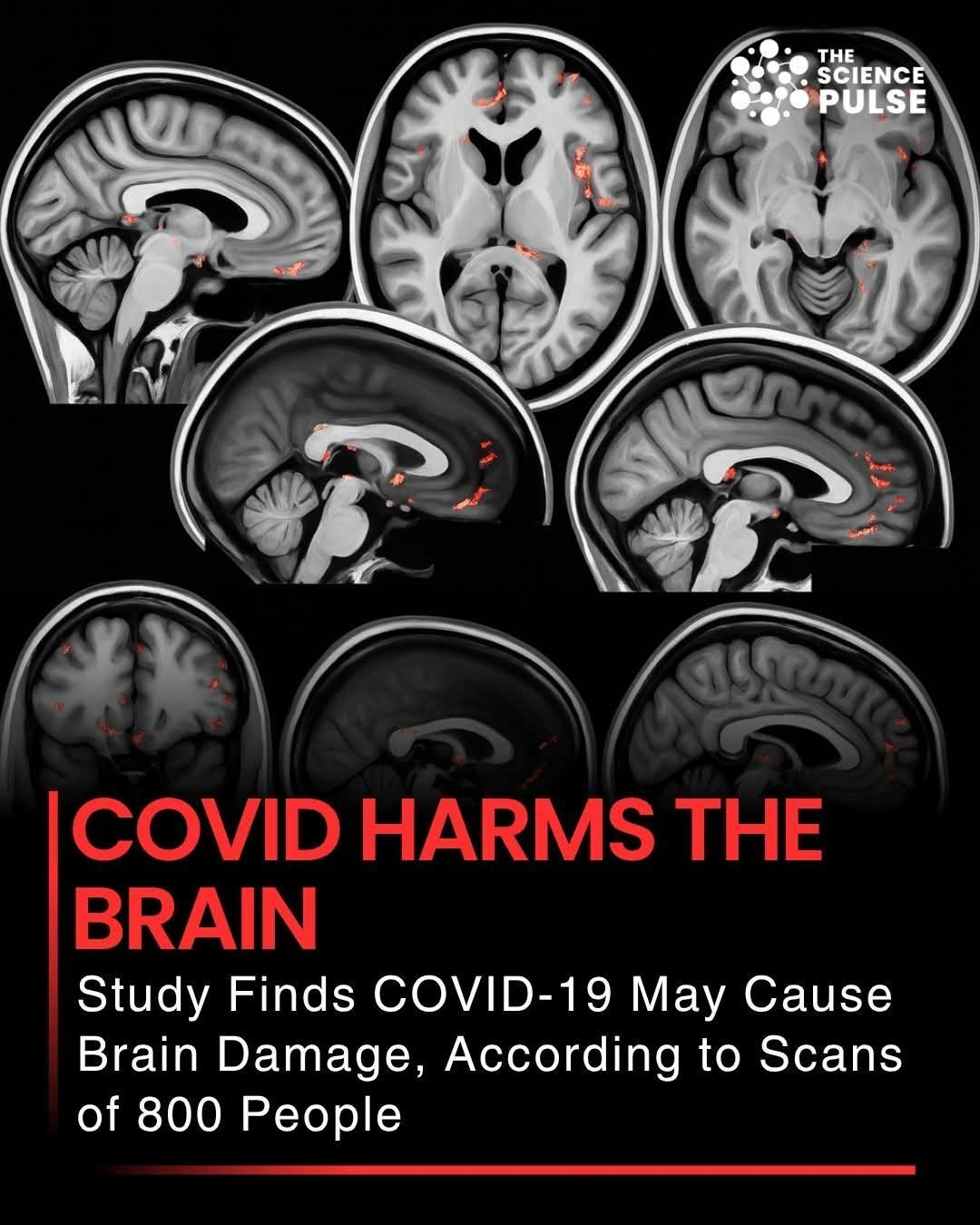
A major new study reveals that COVID-19 can cause measurable brain damage, even in individuals with mild or moderate symptoms. Scans of 800 people showed reductions in gray matter, brain volume, and cognitive function, highlighting the lasting neurological impact of the virus.
Researchers found that COVID can affect areas responsible for memory, decision-making, and sensory processing, potentially increasing the risk of long-term cognitive issues. This study underscores the importance of vaccination, early treatment, and ongoing monitoring for neurological health in COVID survivors.
Even after recovery, some patients may experience brain fog, difficulty concentrating, and slower thinking, indicating that the virus can leave a lasting imprint on the nervous system. Experts urge continued research to understand how to protect and repair brain health following COVID infections.
These findings are a powerful reminder that COVID-19 is not just a respiratory illness but a disease with serious neurological consequences, reinforcing the need for caution, prevention, and awareness.
Long recovery, brain damage, effect of stressors with long COVID
For some, a long road to recovery
French researchers published a new study in JAMA Network Open on 1-year rates of long COVID among 53,047 adults in three population-based groups who took a nationwide survey from Apr 1 to Jun 30, 2020. The researchers obtained blood samples for serologic confirmation of infection from May 1 to Nov 30, 2020, and fielded an online follow-up questionnaire from Jun 1 to Sep 30, 2021. Average participant age was 50.9 years, and 63.7% were women.
In total, 3,972 people had tested positive for SARS-CoV-2, with 2,647 (66.6%) of them reporting at least one symptom during their infections. Of the 2,647 participants, 32.5% said they had at least one COVID-19 symptom for 2 months or longer.
The estimated proportion of participants who had at least one lingering symptom was 18.4% at 6 months, 10.1% at 12 months, and 7.8% after 18 months. Among participants who had symptomatic infections, an estimated 33.6% had more than five symptoms 1 week after infection, falling to 2.8% at 2 months.
An estimated 97.5% of participants with weakness, 94.2% of those with impaired attention or concentration, and 77.5% of those with memory loss reported symptom resolution at 1 year.
The most common long-COVID symptoms were shortness of breath (26.5%), joint pain (26.9%), loss of smell or taste (27.0%), weakness (20.6%), impaired attention or concentration (22.3%), memory loss (40.0%), and sleep disorders (36.6%).
Risk factors for lingering symptoms were age older than 60 years (hazard ratio [HR], 0.78), female sex (HR, 0.64), a history of cancer (HR, 0.61) or tobacco use (HR, 0.80), obesity (HR, 0.75), and more than four symptoms during infection (HR, 0.43).
In general, women were slower to recover their sense of taste or smell. Older people, women, and those with a history of anxiety or depression, cancer, diabetes, tobacco use, obesity, or a higher number of acute symptoms were slower to recover from weakness. Slow resolution of impaired attention or concentration was tied only to older age.
“Given the high level of cumulative incidence of COVID-19, the absolute prevalent number of people with persistent symptoms is a public health concern,” the authors wrote. “These findings suggest the need to optimally manage comorbid conditions in individuals with long COVID to help reduce the duration of their symptoms.”