You sometimes hear fibromyalgia referred to as a “fad diagnosis” or “new disease,” but the truth is that fibromyalgia is far from new. It has centuries of history, with multiple name changes and discarded theories along the way.
While it hasn’t always been accepted by the medical community, and today its acceptance isn’t universal, fibromyalgia has come a long way and current research continues to offer proof that it’s a very real physiological illness.
The most often cited historical account of fibromyalgia comes from a 2004 paper by researchers Fatma Inanici and Muhammad B. Yunus. This history was compiled from their work as well as new information from the past decade. (All sources are cited at the end of the article.)
Back to the Beginning – 1592-1900
Early on, doctors didn’t have separate definitions for all the pain conditions we recognize today. Descriptions and terminology started out broad and gradually narrowed down.
In 1592, French physician Guillaume de Baillou introduced the term “rheumatism ” to describe musculoskeletal pain that didn’t originate from injury. This was a broad term that would have included fibromyalgia as well as arthritis and many other illnesses. Eventually, doctors began to use “muscular rheumatism” for painful conditions that, like fibromyalgia, didn’t cause deformity.
Two hundred years later, definitions still were rather vague.
Love Your Heart This February
The heart is one of the body’s most important organs, powering everything we do. In partnership with Cleveland Clinic, here’s what to know for heart-healthy living.
However, in 1815, Scottish surgeon William Balfour noted nodules on connective tissues and theorized that inflammation could be behind both the nodules and pain. He was also the first to describe tender points (which would later be used to diagnose fibromyalgia.)
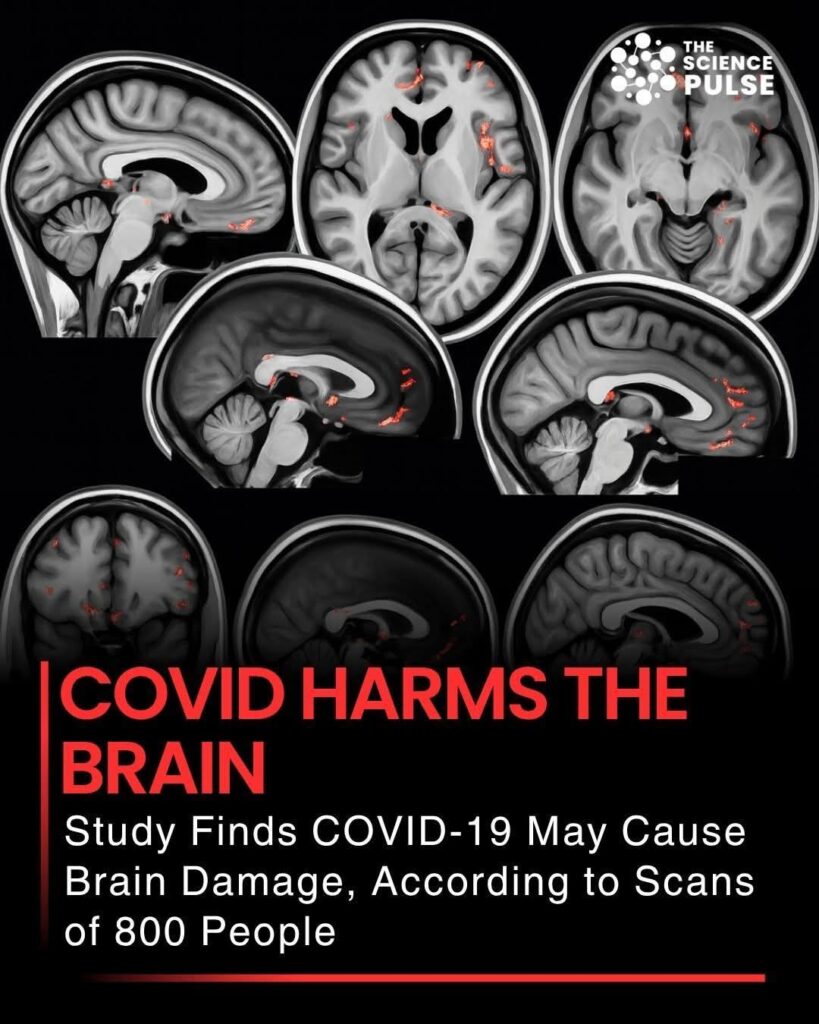
the brain;
1999 – First study demonstrating genetic component to explain why it runs in families;
2000 – Review of evidence coins the term central sensitization syndromes;
2005 – American Pain Society releases first guidelines for treating fibromyalgia pain;
2007 – Lyrica (pregabalin) becomes the first FDA-approved treatment in the U.S. (Cymbalta (duloxetine) and Savella (milnacipran) followed, in 2008 and 2009, respectively;)
2010 – American College of Rheumatology releases alternate diagnostic criteria using questionnaires instead of tender points.
Research has continued to shore up these findings as well as suggest new possible causal factors and mechanisms. As of early 2014, some lines of inquiry include:
Inflammation of the fascia: Some research has suggested that the widespread pain of fibromyalgia may indeed be inflammatory but in the extremely thin body-wide web of connective tissue called fascia.
Extra nerves on blood vessels: A much-publicized study shows extra temperature and pain-sensing nerves in the circulatory system.
Small-fiber neuropathy: Emerging research is showing that certain specialized nerves may be damaged.
Immune System Abnormalities: Some lines of research are showing abnormal activity in the immune system that may suggest chronic immune-system activation or autoimmunity. One study suggests an autoimmune reaction to serotonin. Another proposes a possible diagnostic test based on an immune profile.
Several researchers also are working to establish subgroups of fibromyalgia, believing that it’s the key to nailing down the underlying mechanisms and best treatments. More treatments are always under investigation, and a major goal has long been identifying and establishing objective diagnostic tools such as a blood test or scan. Fibromyalgia still has not found universal acceptance in the medical community, but it’s closer than ever. As research continues to demonstrate that it’s both real and physiological, this condition gains credibility and those of us with it gain understanding, respect, and, most importantly, better treatment options so that we can reclaim our futures.